Presenters
- Sarah Sanders, PhD, Postdoctoral Psychology Fellow, Alaska Family Medicine Residency/Providence Family Medicine Center, Anchorage, AK
- Erin Iwamoto, PsyD, Behavioral Scientist, Alaska Family Medicine Residency/Providence Family Medicine Center, Anchorage, AK
- Virginia Parret, PhD, Behavioral Health Faculty, Licensed Psychologist, Alaska Family Medicine Residency, Anchorage, AK
Summary
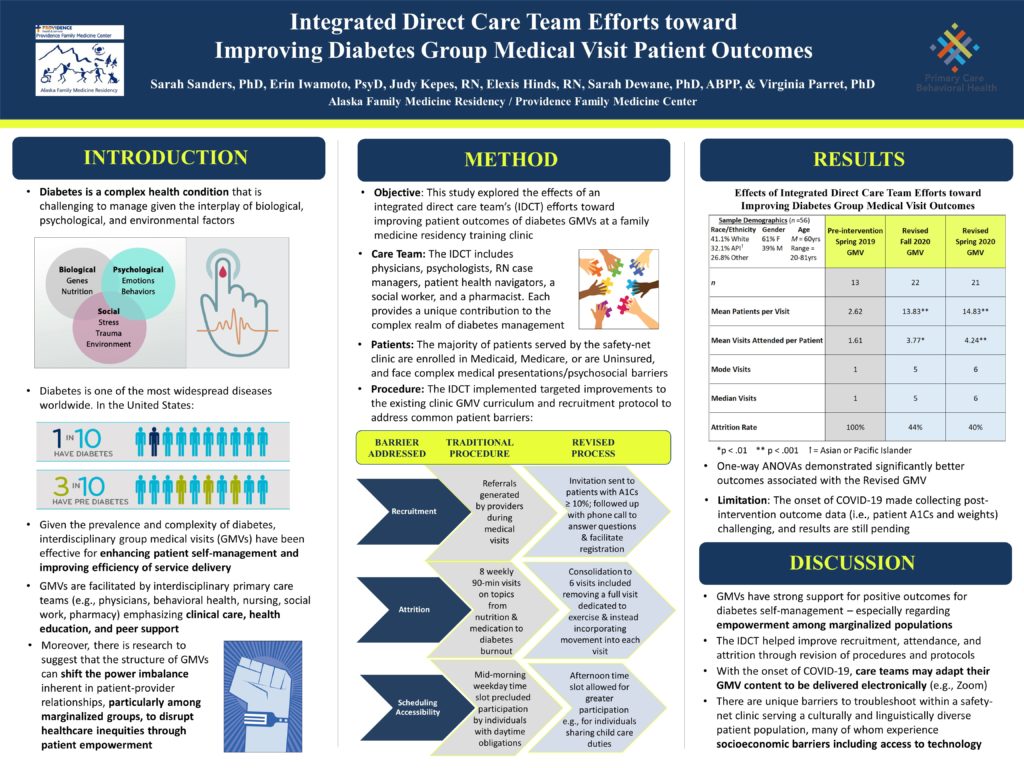
Diabetes is a complex condition that is challenging to manage given the interplay of biological, psychological, and environmental factors. The CDC (2020) found that more than 1 in 10 Americans experience diabetes, and 1 in 3 meet criteria for prediabetes. Given the prevalence and complexity of the disease, group medical visits (GMVs), facilitated by interdisciplinary primary care teams emphasizing clinical care, health education, and peer support, have been effective for patient self-management and improving efficiency of service delivery. Moreover, there is research to suggest that the structure of GMVs can shift the power imbalance inherent in patient-provider relationships, particularly among marginalized groups, to disrupt healthcare inequities through patient empowerment. This study explored the effects of an integrated direct care team’s (IDCT) efforts toward improving patient outcomes of diabetes GMVs at a family medicine residency training clinic. The IDCT includes physicians, psychologists, RN case managers, patient health navigators, social work, and pharmacy. The majority of patients served by the safety-net clinic are enrolled in Medicaid, Medicare, or are uninsured, and face complex medical presentations and psychosocial barriers. Targeted improvements to the existing GMV curriculum and protocol were implemented by the IDCT to address common patient barriers. Improvements included a revised recruitment protocol, consolidation of the curriculum from 8 visits down to 6, and offering an afternoon time slot. Preliminary data from a between-groups design with 54 participants, 63% women, ages 20 to 81 years old, demonstrated statistically and clinically significant improvements in GMV attendance and attrition after implementation of the targeted improvements. Data collection (i.e., post-intervention patient weights and A1Cs) is ongoing, and ANOVAs to determine effectiveness of the GMV intervention are pending, with results to be discussed.
Objectives
- Describe the benefits of a group medical visit in the context of diabetes management
- Identify the value of integrated direct care team member involvement in recruitment, design, and implementation of the group medical visits
- Understand the improvements in patient outcomes associated with group medical visits coordinated and delivered by an integrated direct care team

Leave a Reply